Pre and post-procedure care for hip replacement
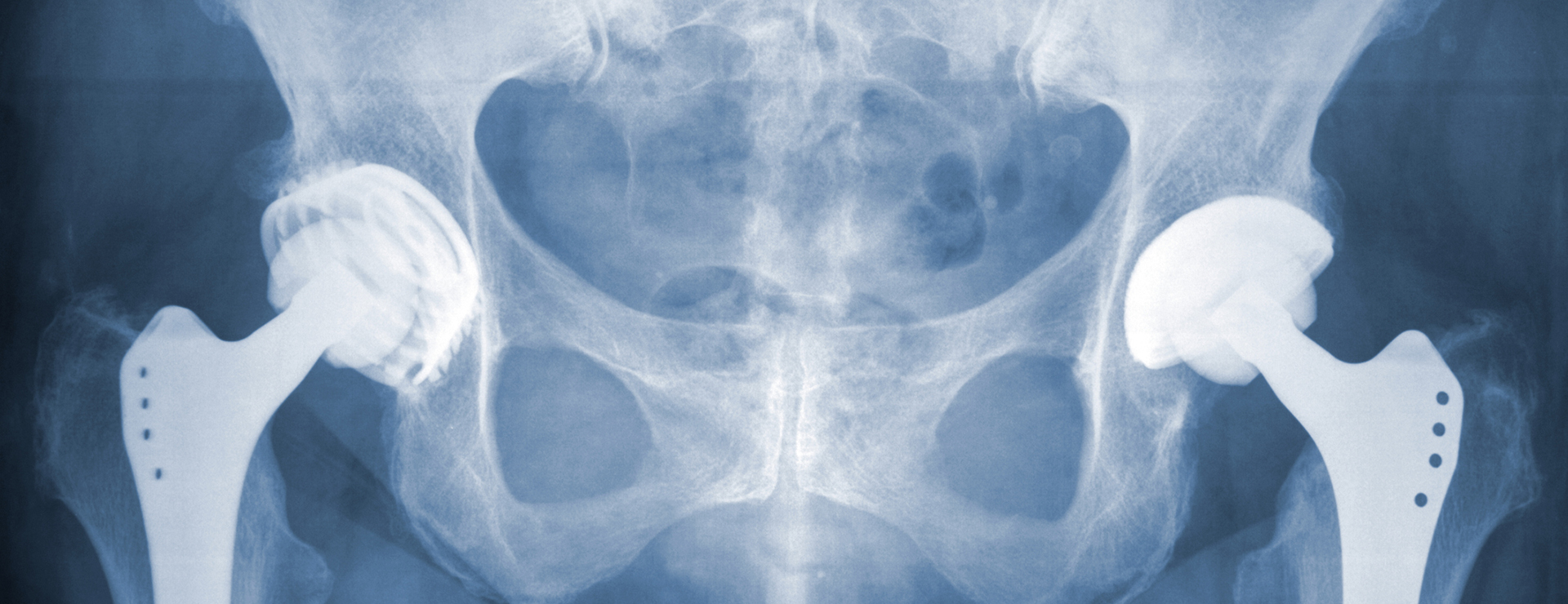
Hip replacement is a surgery where a damaged portion of your hip is removed. Your doctor replaces the damaged hip with new prosthetic parts. These parts are normally formed by metal, very hard plastic, or ceramic. The surgery also called total hip replacement or total hip arthroplasty. The purpose of the replacement is to reduce pain and improve functioning.
There can be many underlying reasons which lead to the need for hip replacement. Injuries, medical conditions like arthritis caused by regular wear and tear or an overactive immune system that erode cartilage or inadequate supply of blood to the ball are some common reasons. Many symptoms indicate that you should consider replacement surgery. If you have constant pain despite medication that interferes with walking and sleeping, you should go for the replacement. Additionally, you may feel difficulty rising from a sitting position or going up and down the stairs.
The surgery is a common but delicate procedure. You need to take proper care before and after the surgery to avoid any complications.
- Pre-procedure preparation
Preparation is a collective effort from you and your surgeon. Your surgeon will do the primary examination for evaluating your medical history and present medication. He will examine your hip and check the motion range and muscle strength. A general physical examination is conducted to ensure that you are ready for the surgery. Some blood tests, x-rays, and MRI may be also needed. This time is an opportunity to ask your surgeon, details of the surgery. You should inquire about the medication to be stopped or continued before the procedure.
- Post-procedure care
Right after the surgery, the medical team will monitor your blood pressure, pulse rate, and alertness. They will evaluate your condition and provide the necessary medication.
- Blood clot prevention
After surgery, there is a risk of blood clotting in your leg. You will be encouraged to stay mobilized and wear compression stockings for pressure applications. You may be given blood-thinning medications if needed.
- Physical therapy
Physical therapy is an essential part of recovery. It starts the very next day of the surgery. It involves exercises that help you to regain joint and muscle usage. The exercises aim to increase strength in your muscles and improve mobility. You can gradually increase the pressure on your leg. It also helps you learn, how to walk with walkers, crutches, or cane.
- Follow-up care and recovery
Once you are at home, you have to have somebody to take care of. Your doctor may give some instructions or tips to your caregivers regarding movements and diet. You should take a protein and fiber-rich diet. It is important to consider come modifications at home. You may have to get a raised toilet seat. You should keep everything that you may need at the waist level. This helps in avoiding the need to bend down. Keep the exercise a part of your routine even at home. You may have to make follow-up appointments with your surgeon to monitor the healing process. It may take around 6 to 12 months for a full recovery and resuming regular movements.
